A 60 year old woman, housewife by occupation presented with the complaints of
Dyspnea on exertion since 6 months
She was apparently asymptomatic 6 months back after which one day after getting up in the morning she suddenly started to experience dyspnea, which progressed over the next 3 days. She says the dyspnea aggravated on walking and on laying down in supine posture, she says her dyspnea reduced in sitting posture. Because of this she started to have disturbed sleep. The following day she experienced retrosternal chest pain radiating to her left shoulder. Over the next 3 days she had intermittent episodes of chest pain on and off along with productive cough with scanty frothy, non foul smelling, non blood tinged sputum.
She got admitted with us 6 months back with these complaints for 1 week and was diagnosed with heart failure with reduced ejection fraction of 29%, secondary to coronary artery disease, Iron deficiency anemia and has been on regular medications ever since.
Since the past 6 months, she says she still feels dyspnoeic on walking for even 5 minutes and since the past 2 days she has again started to experience intermittent retrosternal chest pain radiating to her left shoulder. On further questioning, she also says she has bendopnea, feeling dizzy on exertion and also heavy palpitations on exertion. She denies cold sweats but has nocturia occasionally.
Past History
She has had three vaginal deliveries and was tubectomised 35 years back.
She was also diagnosed to be a hypertensive and diabetic 10 years back on a routine check up and has been using Tab Telma Beta 40/50mg, once daily along with Tab Metformin 500mg once daily since the past 10 years.
Along with this she has been taking Tab Ultracet occasionally for her lower back pain along with a spinal brace for her lower back pain.
Since the past 6 months she has also been on Tab Lasix 40mg, twice daily along with Tab Orofer XT, once daily.
Personal history
She has been experiencing loss of appetite since the past 6 months. She consumes a mixed diet. She has no complains regarding her bowel and bladder habits or sleep.
Family history
No significant family history
ON GENERAL EXAMINATION:
She was conscious, coherent and cooperative
Pulse rate - 75 beats per minute, regular, normal in volume with no radio-radial or radio-femoral delay.
Blood pressure - 110/70mmhg, right arm, in supine posture
Respiratory Rate - 18 cycles per minute
Spo2 - 98% on Room Air
GRBS - 150mg/dl
JVP - Not raised
HEAD TO TOE GENERAL EXAMINATION:
Weight - 55 kgs
Thin built
Hair - Thin and graying +
Eyes - Pallor +, No icterus
Nails - No clubbing, No Koilonychia
No spinal deformities
Legs- No pedal edema
SYSTEMIC EXAMINATION:
Cardiovascular Sytem:
Inspection:
Shape of the chest - Ellipsoid
Breast abnormalities - Absent
Cutaneous lesions - Absent
No dilated veins, scars or visible pulsations
Palpation:
Apex beat present in 6th ICS in Midclavicular line
No palpable pulsations in aortic and Pulmonary areas
No palpable pulsations in sternoclavicular area
No left parasternal pulsations
No epigastric pulsations palpable
Auscultation:
Muffled S1,S2 +
Pansystolic murmur +
Respiratory system:
Inspiratory crepts in right IAA and ISA
Per Abdomen:
Soft
No tenderness
No guarding, rigidity
Bowel sounds present
Central Nervous System Examination:
Normal
Provisional Diagnosis:
1. HEART FAILURE WITH REDUCED EJECTION FRACTION - 29%
2. IRON DEFICIENCY ANEMIA
3. KNOWN CASE OF HYPERTENSION AND DIABETES MELLITUS SINCE 10 YEARS
REPORTS:
ECG:
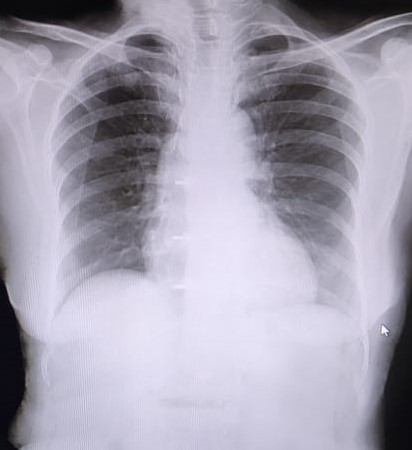
Chest X Ray PA view:
Complete Blood Picture:
Hemoglobin - 8.5 g/dl
TLC - 8000 cells/cumm
Platelets - 1.5 Lakhs/cumm
Peripheral smear - Anisopoikilocytosis with hypochromasia microcytes and pencil forms
ABG:
Ph - 7.45
PCO2 - 35.5mmhg
PO2 - 92mmhg
HCO3 - 24.6 mmol/l
Complete Urine Examination:
No abnormalities present
Renal Function test:
Serum creatine - 0.8mg/dl
Blood urea - 30mg/dl
Serum Sodium - 138 meq/l
Serum potassium - 4.5 meq/l
Serum Chloride- 100 meq/l
Liver function test:
Total bilirubin - 0.46mg/dl
Direct bilirubin - 0.16 mg/dl
AST - 10 IU/L
ALT - 11 IU/L
ALP - 163 IU/L
Total proteins - 5.4 gm/dl
Albumin - 3.5 gm/dl
RBS - 157mg/dl
FBS - 137 mg/dl
PLBS - 264 mg/dl
HbA1c - 6.6 %
Reticulocyte count - 2%
Serum Ferritin - 12 ng/mL
2DECHO:
Global Hypokinesia, Mild LVH
Mild MR +, Trivial TR +/ AR+
Sclerotic AV
AML Doming
EF = 29% , RSVP = 29 mmhg
No PAH
Severe LV Dysfunction
Minimal PE
Diastolic Dysfunction +
TREATMENT:
1. Tab Lasix 40mg/PO/BD
8am and 4pm
2. Tab Telma Beta 40/50mg PO/OD
8am
3. Tab Metformin 500mg/PO/OD
8am
4. Tab Orofer XT/PO/BD
5. Tab Isosorbide Dinitrate 5mg/PO/BD for 3 days
6. Syrup Lactulose 10ml/PO/BD
7. Fluid Restriction <1 Litre/day
8. Salt Restriction 2 grams/day
9. Strict diabetic diet - was advised to follow Harvard plate.
Sourced from - Here


Comments
Post a Comment
Your inputs are welcome :)